With so many adults and students working from home right now, DIY home-office setups are becoming the new standard for workspaces.
One thing is for sure: we have seen a surge in number of people with posture related issues from long days of zoom calls while hunched over a kitchen table.
What Can Physical Therapy Do to Help?
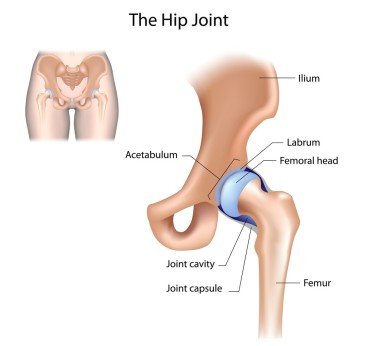
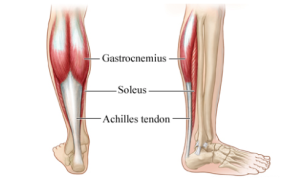
Poor posture can lead to a whole host of issues including (but certainly not limited to) neck pain, back pain, carpal tunnel disorder, hip impingement, and headaches. Physical therapists are trained to treat many different disorders that can result from poor posture, and can provide skilled advice on how to modify your office and desk to keep your body aligned. Treatment options often include joint mobilizations, personalized stretching programs, traction, postural training, and nerve mobilizations to help relieve tension.
Seeking Ergonomic Advice?
At Active Marin Physical Therapy, our therapists are trained to provide skilled and personalized ergonomic assessments. We are available for both in-person and telehealth consultations. Online telehealth consultations are a perfect match for ergonomic evaluations because it allows the physical therapist to see you in your natural environment at your desk. Contact us to set up a consultation.
5- Step Ergonomic Checklist
How do you know if your home-brew desk setup is setting you up for success? Here are the basic elements to check:
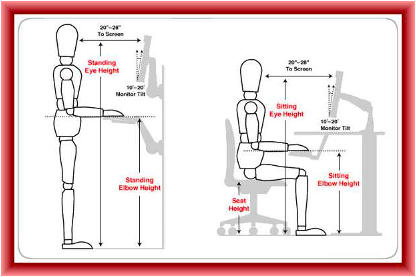
1. Is your computer screen at eye level?
It is essential that your computer is at eye-level in order to avoid neck and shoulder pain. If you have a desktop computer, consider using a computer stand or adjustable computer mount to raise your screen to eye level. If you are using a laptop or an ipad, prop your device up on an elevated laptop stand– it can make a huge difference. If you also need to do a lot of typing on your device, you may consider getting a wireless keyboard and mouse to set under your laptop stand so that both your neck and arms can be in a comfortable position while using your laptop or iPad.
2. Does your chair support your low back?
Many office workers find that a chair with lumbar support helps ease their back pain. If your chair does not have lumbar support, try placing a rolled up towel or a lumbar support roll behind your lower back for extra support. A cushioned seat pad can also help relieve pain and distribute forces when you are sitting in a firm chair all day.
3. Are your legs parallel to the floor?
The ideal situation is to have a chair that is height-adjustable so that your thighs can be parallel to the floor with your feet flat on the ground. If you cannot adjust the height of your chair, and your feet do not reach the ground, consider using a footrest to set your feet on.

4. Are your hands at the same height as your elbows?
Whether you are using a sitting or a standing desk, the ideal desk height is one where your hands are at or slightly below your elbow level when you are using your keyboard. If your desk is too low, place sturdy books or boards under the desk legs to raise the height of the table. If your desk is too high, you can use a keyboard tray that allows you to use your keyboard below the top of your desk. If you are able to invest more money in your desk set-up, a sit-to-stand desk can be a good ergonomic option that prevents back pain.
5. Are you frequently looking down at paper on your desk?
If you are frequently referencing written notes while using your computer, you should consider using a document holder which allows you to prop up your notes next to your computer. There are many low-cost options for document holders, and they can save your neck a lot of pain from being bent over all day long.
Have more questions or want personalized assistance? Contact us to set up an in-person or telehealth ergonomic consultation.


 Olympic athletes have trained their bodies to near perfection by the time they arrive in PyeongChang for the 2018 Olympics. However it is the mental preparation for the pressure that comes with competing at the 2018 Olympics that is critical, and may ultimately determine a gold versus silver medal. Visual imagery has long been a part of the training regimen of elite athletes and has become increasingly more utilized across the world.
Olympic athletes have trained their bodies to near perfection by the time they arrive in PyeongChang for the 2018 Olympics. However it is the mental preparation for the pressure that comes with competing at the 2018 Olympics that is critical, and may ultimately determine a gold versus silver medal. Visual imagery has long been a part of the training regimen of elite athletes and has become increasingly more utilized across the world.