Osteoarthritis
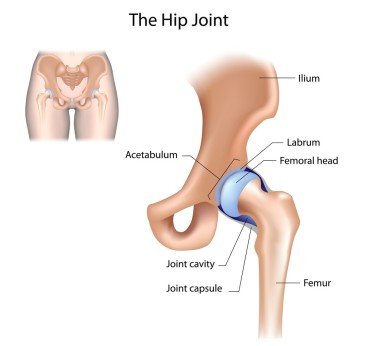
Osteoarthritis (OA) is the most common cause of hip pain in adults over 50. Simply put, OA is a degeneration of the hip joint. The cartilage that lines the joint degenerates over time until the femur (ball) and the acetabulum (socket) no longer have the lubrication and protection required for normal, smooth joint motion. This can become quite painful and ultimately lead to decreased activity levels and increased difficulty with daily tasks such as walking and standing up, especially first thing in the morning.
Treatment for hip OA can include stretching and strengthening of the muscles surrounding the hip. Ultrasound and hot packs can be used in the short-term management of pain and activity limitations in order to return to exercise and begin therapy quicker. Manual therapy including joint mobilization, soft tissue release and massage all have significant evidence supporting their use to improve function and reduce activity limitations in people with OA.
2017 updated risk factors for osteoarthritis of the hip include, but are not limited to:
- Decreased hip internal rotation and flexion range of motion
- Morning stiffness
- Male sex
- Higher BMI
- Hip pain
- Age over 50
Hip Internal Rotation : range of motion becomes limited
Hip Flexion also becomes restricted and painful
We’re here to help. In many cases, a prescription of manual therapy to improve hip range of motion, as well as an individualized exercise program can help to prolong or prevent joint replacement surgery.
Treatment recommendations include:
- Ultrasound for short-term pain reduction
- Flexibility, strengthening and endurance exercises
- Manual therapy for joint mobility, flexibility and pain
- Education on activity modification, exercise, supporting weight reduction when overweight, and methods of unloading arthritic joints.
Recent evidence suggests that NSAIDs (such as Aspirin and ibuprofen), COX-2 inhibitors, and steroid injections are effective at relieving pain and symptoms in hip OA. However, there is some evidence that suggests NSAIDs may increase the progression of hip OA my decreasing glycosaminoglycan synthesis. In addition, there can be serious gastrointestinal side effects associated with NSAID use. Consult your physician before use.
What can you do at home?
Below is a video with a few stretches recommended to improve hip mobility. This is not an exhaustive list but rather a starting point and something to try. It is always recommended that you see a physical therapist to individualize your treatment approach.
The information provided is not medical advice. If you would like more information please visit us at www.ActiveMarin.com or call to schedule an appointment.